Questions
What was the mental health scene like in 2010 for those at the grittier end of the stick? What was 2010 like for people in secondary care? For people under community mental health teams?
Was there more recovery in 2010? Were people in secondary care able to access mainstream in 2010? Were they less doomed to what Dr. Pat Deegan calls 'a career in mental health'?
Did people with severe and enduring mental health conditions receive enough support from services? Did they receive the right support? Did the support help them or hinder them?
Some answers
Throughout 2010, statutory and voluntary services responded to the health challenge of independence and mainstream in several key ways. Firstly, mental health teams set up some important initiatives. These were geared towards client independence and recovery. Many predominantly service-user led.
Recovery University in the south-west London borough of Merton enables secondary care clients to access a wide spectrum of trainings and skillsets. These include preparing for work, independence and life skills, confidence building, anger management and many more. Recovery University also trains service users as trainers for forthcoming courses.
Other community initiatives are also up and running, including wellbeing programmes and access to psychological therapies. However, pyschological therapies in non-clinical settings are still not available should you happen to have a severe and enduring mental health condition.
Training the trainers often draws upon experiences and qualifications which service users have already gained within their life journeys. Mainstream groups have also utilised service user skills as part of their own training programmes in areas such as visual arts, music and creative writing. This has taken the recovery university one stage further, providing paid employment and access to mainstream.
Statutory services continued to have success in keeping people out of hospital or limiting hospital stays to a minimum. The downside of this is that more and more people are being discharged from statutory services altogether. In 2011 this will inevitably result in more pressure on GP services, as it is these practitioners who will become responsible under the latest government directives.
The rolling-out of the personalisation programme should mean more access to direct payments for many clients under mental health care plans. It should also mean more and more creative uses of direct payments, as DP is being promoted for any activity or outcome that a client deems relevant to his or her recovery. The Personal Stories videos on the NMHDU site bears witness to some of these outcomes. With more and more people being discharged from mental health services, it is crucial that personalisation is a success in the new year.
An ongoing series of articles on themes of social inclusion. More details of John's work and training schedules can be found at www.mhfatrainings.com MHFA England is the national licensed organisation for MHFA UK (www.mhfaengland.org.uk)
Tuesday 21 December 2010
Friday 10 December 2010
UK Mental Health Review of the Year 2010 - part 1
The background
Most years are momentous for mental health and 2010 has been no exception.
Momentous for individuals experiencing mental health conditions or their onset. Momentous for their family, friends and carers. Momentous for the way that society, the legislature and the populace have chosen to respond to the challenge of mental health.
There has been a clear road, a visible highway. The 2005 amendments to the Disability Discrimination Act (DDA) have been taken further with the Equality Act that came into force on October 1st 2010. Carol Black's 2008 report 'Working for a Healthier Tomorrow' was a round-up and reinforcement of the initiatives embodied in DDA, designed to address key concerns of health and legal rights in the workplace.
The year 2010
Major businesses and business organisations have also addressed the massive loss to the economy and to human happiness that can be caused by mental ill-health. In 2005 the Confederation of British Industry was concerned enough to commission its own research. Business owners and directors have not been slow to follow their confederation's lead.
Supported by business ‘dragon’ Duncan Bannatyne, Mind’s ‘Taking care of Business’ campaign continues to highlight the initiatives being taken by many employers around issues of mental health at work. Some of the companies who signed up to support the Mind campaign include EDF energy, BT, Hewitt Consultancy, AXA and police and security services. Hewitt Associates helped set up an Employee Assistance programme allowing staff access to counselling services where appropriate.
Anti-stigma group Shift is also 'high visibility' in its tireless campaigning for an end to mental health discrimination and in its promotion of understanding the need to support good mental health in the workplace.
Equality Act
The increasing awareness of how mental health affects culminated in 2010 with the Equality Act. The Act reinforces all the implementations of the Disability Discrimination Act (DDA) and in particular, the rights of employees who have disclosed a mental health condition. Before the act came into force, employees had the legal right to reasonable adjustments in their working conditions where appropriate. With the Equality Act, the burden of proof now lies with the employer to show that adjustments have been made rather than with the employee to prove they haven't. It is a highly significant rights-based change.
Most years are momentous for mental health and 2010 has been no exception.
Momentous for individuals experiencing mental health conditions or their onset. Momentous for their family, friends and carers. Momentous for the way that society, the legislature and the populace have chosen to respond to the challenge of mental health.
There has been a clear road, a visible highway. The 2005 amendments to the Disability Discrimination Act (DDA) have been taken further with the Equality Act that came into force on October 1st 2010. Carol Black's 2008 report 'Working for a Healthier Tomorrow' was a round-up and reinforcement of the initiatives embodied in DDA, designed to address key concerns of health and legal rights in the workplace.
The year 2010
Major businesses and business organisations have also addressed the massive loss to the economy and to human happiness that can be caused by mental ill-health. In 2005 the Confederation of British Industry was concerned enough to commission its own research. Business owners and directors have not been slow to follow their confederation's lead.
Supported by business ‘dragon’ Duncan Bannatyne, Mind’s ‘Taking care of Business’ campaign continues to highlight the initiatives being taken by many employers around issues of mental health at work. Some of the companies who signed up to support the Mind campaign include EDF energy, BT, Hewitt Consultancy, AXA and police and security services. Hewitt Associates helped set up an Employee Assistance programme allowing staff access to counselling services where appropriate.
Anti-stigma group Shift is also 'high visibility' in its tireless campaigning for an end to mental health discrimination and in its promotion of understanding the need to support good mental health in the workplace.
Equality Act
The increasing awareness of how mental health affects culminated in 2010 with the Equality Act. The Act reinforces all the implementations of the Disability Discrimination Act (DDA) and in particular, the rights of employees who have disclosed a mental health condition. Before the act came into force, employees had the legal right to reasonable adjustments in their working conditions where appropriate. With the Equality Act, the burden of proof now lies with the employer to show that adjustments have been made rather than with the employee to prove they haven't. It is a highly significant rights-based change.
Friday 26 November 2010
Wednesday 17 November 2010
Are UK services ready for the personalisation programme?
Within two years, by 2013, the Personalisation Programme is set to be rolled out across UK health and mental health services.
In June 2010 Eight Primary Care Trusts began roadtesting direct payments for personal health budgets.
'Patients will be offered more choice and control over their healthcare' announced Care Services minister Paul Burstow. 'The launch of the first direct payment scheme is an important step towards putting patients at the heart of everything the NHS does' he added .
The Coalition government has pledged its 'commitment to extend access' to direct payments. As Paul Burstow reasons, direct payments 'is a step away from the rigidity of the Primary Care Trusts deciding what services a patient will receive'.
Quite how the PCTs are going to be less rigid with their budgets is still unclear. Some formidable outcomes have already been achieved in some of the areas where the scheme is being piloted ( testimonial videos at NMHDU). Nonetheless, the PCTs are still holding the budgets for direct payments. Where direct payments is not being piloted or simply not understood, patients and carers are still being denied their rights. The 'rigid' approach is still being applied and clients wishing to access mainstream activities of their own choice are being turned down.
The Care Services minister has announced that direct payments 'will stop healthcare from slipping back to the days of one-dimensional, like-it-or-lump-it services'.
It is a great pity and possibly a legal scandal that clients wishing to determine their own recovery journeys are still being turned down by PCTs for direct payments.
'One-dimensional, like-it-or-lump-it services' are still around.
In June 2010 Eight Primary Care Trusts began roadtesting direct payments for personal health budgets.
'Patients will be offered more choice and control over their healthcare' announced Care Services minister Paul Burstow. 'The launch of the first direct payment scheme is an important step towards putting patients at the heart of everything the NHS does' he added .
The Coalition government has pledged its 'commitment to extend access' to direct payments. As Paul Burstow reasons, direct payments 'is a step away from the rigidity of the Primary Care Trusts deciding what services a patient will receive'.
Quite how the PCTs are going to be less rigid with their budgets is still unclear. Some formidable outcomes have already been achieved in some of the areas where the scheme is being piloted ( testimonial videos at NMHDU). Nonetheless, the PCTs are still holding the budgets for direct payments. Where direct payments is not being piloted or simply not understood, patients and carers are still being denied their rights. The 'rigid' approach is still being applied and clients wishing to access mainstream activities of their own choice are being turned down.
The Care Services minister has announced that direct payments 'will stop healthcare from slipping back to the days of one-dimensional, like-it-or-lump-it services'.
It is a great pity and possibly a legal scandal that clients wishing to determine their own recovery journeys are still being turned down by PCTs for direct payments.
'One-dimensional, like-it-or-lump-it services' are still around.
Care and Support - can they hinder recovery?
Care and support are not the only models or frameworks for mental health recovery. The establishing or re-establishing of what Dr. Pat Deegan refers to as 'valued social roles' can be held back by a mental health system that often encourages the client to choose 'a career in mental health' (Pat Deegan).
A career in mental health means living longterm on benefits and longterm marginalisation from mainstream life. A career in mental health will identify symptoms, diagnoses, medication and team support but will often leave out aspirations, goals, priorities.
Where access to mainstream is encouraged, it can often be through projects or programmes which take place in special settings or are designed for people with mental health conditions. So the marginalisation continues.
A genuine return to mainstream can only take place in mainstream. This is where the role of the bridge builder comes in. A client who has worked with a mainstream bridge builder identifies goals and priorities for him or herself. It is the bridge builder's job to signpost or link the client up with mainstream venues appropriate to the client's life choices. The amount of support a client may request from there on is determined only by the client.
A career in mental health means living longterm on benefits and longterm marginalisation from mainstream life. A career in mental health will identify symptoms, diagnoses, medication and team support but will often leave out aspirations, goals, priorities.
Where access to mainstream is encouraged, it can often be through projects or programmes which take place in special settings or are designed for people with mental health conditions. So the marginalisation continues.
A genuine return to mainstream can only take place in mainstream. This is where the role of the bridge builder comes in. A client who has worked with a mainstream bridge builder identifies goals and priorities for him or herself. It is the bridge builder's job to signpost or link the client up with mainstream venues appropriate to the client's life choices. The amount of support a client may request from there on is determined only by the client.
Wednesday 10 November 2010
Equalities Act 2010
During the parliamentary stages of the Equality Bill, mental health organisation Mind lobbied with other mental health and disability charities to get a ban on pre-employment questionnaires included in the Act. After securing cross-party support for the principle of a ban on questions that ask about a candidate's medical history and putting considerable pressure on Ministers, the last Government introduced a new clause to the Equality Bill making these questions unlawful.
The Equality Act came into force on October 1st 2010. The act bans companies from finding out whether potential employees are healthy enough to work for them prior to an offer of employment. Candidates will no longer be expected to declare medical issues during the recruitment stage unless it is specifically related to their job role.
Equality campaigners have long argued that employers discriminate against prospective employees with mental health issues, disabilities or a long history of illness, putting people off applying for a job.
However, 65pc of employers still ask a candidate about their health prior to a job offer, and 48pc ask potential employees to fill out a questionnaire detailing medical conditions and sickness records, according to a poll of 100 companies by law firm Pannone.
Jim Lister, head of employment law at Pannone, said: "The penalties for employers include investigation by the Equality and Human Rights Commission and the reversal of the burden of proof, meaning that the employer will be assumed to have discriminated, unless it can show there was another reason for non-selection.
Organisations that learn of a person's health issue after the job offer but fail to make reasonable adjustments and are forced to withdraw the offer face litigation, lawyers have said.
The reversal of the burden of proof is highly significant. Effectively this means that an employee who feels discriminated against on the grounds of mental ill-health, for example, is not required to prove that this is the case. It becomes the employer's responsibility to prove that this is not the case. If proved otherwise, the employer will be required by law to comply with equalities legislation and where necessary, to make reasonable adjustments on behalf of the employee.
The Equality Act came into force on October 1st 2010. The act bans companies from finding out whether potential employees are healthy enough to work for them prior to an offer of employment. Candidates will no longer be expected to declare medical issues during the recruitment stage unless it is specifically related to their job role.
Equality campaigners have long argued that employers discriminate against prospective employees with mental health issues, disabilities or a long history of illness, putting people off applying for a job.
However, 65pc of employers still ask a candidate about their health prior to a job offer, and 48pc ask potential employees to fill out a questionnaire detailing medical conditions and sickness records, according to a poll of 100 companies by law firm Pannone.
Jim Lister, head of employment law at Pannone, said: "The penalties for employers include investigation by the Equality and Human Rights Commission and the reversal of the burden of proof, meaning that the employer will be assumed to have discriminated, unless it can show there was another reason for non-selection.
Organisations that learn of a person's health issue after the job offer but fail to make reasonable adjustments and are forced to withdraw the offer face litigation, lawyers have said.
The reversal of the burden of proof is highly significant. Effectively this means that an employee who feels discriminated against on the grounds of mental ill-health, for example, is not required to prove that this is the case. It becomes the employer's responsibility to prove that this is not the case. If proved otherwise, the employer will be required by law to comply with equalities legislation and where necessary, to make reasonable adjustments on behalf of the employee.
business,social inclusion
employer,
employment,
equalities act
History of Social Inclusion
Social Inclusion and mainstream arise out of a history and out of a history of ideas.
Government think-tanks in the late 1990s and early 2000s had a key role in developing current thinking and practice around social inclusion. The envisaging of 'social domains' relevant to people's lives arises from these seminal ideas. The role of mainstream bridge builder is also developed around the concept of mainstream as a pathway for mental health recovery.
Social Inclusion goes back even further. A single act of defiance by Rosa Parks in 1955 in Alabama Mississippi. A black woman refusing to give up her seat on the bus to a white person, thereby defying the segregration laws. A key moment that lies at the heart of the civil rights movement, not just for the United States but for equality and social inclusion everywhere.
Equal opportunities, diversity, social inclusion and fairness are now commonplaces, enshrined in the way we strive to live and work today.
Government think-tanks in the late 1990s and early 2000s had a key role in developing current thinking and practice around social inclusion. The envisaging of 'social domains' relevant to people's lives arises from these seminal ideas. The role of mainstream bridge builder is also developed around the concept of mainstream as a pathway for mental health recovery.
Social Inclusion goes back even further. A single act of defiance by Rosa Parks in 1955 in Alabama Mississippi. A black woman refusing to give up her seat on the bus to a white person, thereby defying the segregration laws. A key moment that lies at the heart of the civil rights movement, not just for the United States but for equality and social inclusion everywhere.
Equal opportunities, diversity, social inclusion and fairness are now commonplaces, enshrined in the way we strive to live and work today.
Friday 8 October 2010
How mainstream is roadblocked
For many years mainstream has been perceived and practised as a key component of the care pathway in mental health provision.
At several stages of the pathway into mainstream there are roadblocks. These can occur from the individual client, from services, even from families and carers. An individual can feel apprehensive of stepping over the threshold into mainstream activities. This can be for a variety of reasons, ranging from self-stigma or from being so long in the mental health system that independence seems a very distant option. Contrary to some current opinion, it is not stigma from mainstream society that creates the main roadblock.
Dr. Pat Deegan's belief is that too often the health system can encourage what she calls 'a career in mental health' and nothing else. This viewpoint is based on her experience as a service user and it still holds true.
A great deal is being achieved by service users themselves to challenge the roadblocks. This is particularly true where creative and personalised use of direct payments and individual budgets have really taken off around the UK. It hasn't happened everywhere but some immensely inspiring stories and testimonials can be viewed at the NMHDU website.
Creative use of direct payments in mental health recovery is currently sporadic. The intention was that this should increase towards full implementation of the personalisation programme. Invididual budgets were scheduled to become the engine for much healthcare practice all over the UK by 2013. However, this is now completely overshadowed and possibly lost permanently, in the thrust towards GP consortia and budget management.
Alongside the sudden disappearance of direct payments is the disappearing access to therapies, both for primary and secondary care patients. Secondary care clients have often lost out in the therapies scenario for a variety of reasons. But clients in primary care are still entitled to a reasonably smooth road to psychological therapies. Entitlement does not ensure that those therapy services are available and in practice these too are disappearing along with personalisation and individual budgets.
Of course any client is free to fund their own mainstream recovery pathway and many do. The outcomes in this area alone (south-west London) have often been formidable. A composer who has funded her own recordings and launches now has self-employment through her music. Many are those who have accessed adult education courses and further training. Individuals have re-accessed faith venues which they had previously felt unable to enter for many years.
Not all these initiatives require direct payments - anyway those have now dried up. Many activities are free to access or funded by individual clients from their own pockets. Where direct payment has been needed it has often made the crucial difference.
Third-sector organisations also do great work in promoting access to mainstream through a variety of initiatives. 'Emergence' is an arts group run by and for service users who are also visual artists. In London and around the country 'Emergence' has pioneered access to visual arts as well as giving a platform for creativity and exhibition spaces for artists with personality disorder.
'Imagine' in south west London and Surrey also promotes a variety of arts opportunities including music production and visual arts. These are open to service users but take place in mainstream settings.
Mainstream environments have their own health, safety and insurance policies. As a consumer, the service user to entitled to the protection of these policies along with every other mainstream customer and client.
At several stages of the pathway into mainstream there are roadblocks. These can occur from the individual client, from services, even from families and carers. An individual can feel apprehensive of stepping over the threshold into mainstream activities. This can be for a variety of reasons, ranging from self-stigma or from being so long in the mental health system that independence seems a very distant option. Contrary to some current opinion, it is not stigma from mainstream society that creates the main roadblock.
Dr. Pat Deegan's belief is that too often the health system can encourage what she calls 'a career in mental health' and nothing else. This viewpoint is based on her experience as a service user and it still holds true.
A great deal is being achieved by service users themselves to challenge the roadblocks. This is particularly true where creative and personalised use of direct payments and individual budgets have really taken off around the UK. It hasn't happened everywhere but some immensely inspiring stories and testimonials can be viewed at the NMHDU website.
Creative use of direct payments in mental health recovery is currently sporadic. The intention was that this should increase towards full implementation of the personalisation programme. Invididual budgets were scheduled to become the engine for much healthcare practice all over the UK by 2013. However, this is now completely overshadowed and possibly lost permanently, in the thrust towards GP consortia and budget management.
Alongside the sudden disappearance of direct payments is the disappearing access to therapies, both for primary and secondary care patients. Secondary care clients have often lost out in the therapies scenario for a variety of reasons. But clients in primary care are still entitled to a reasonably smooth road to psychological therapies. Entitlement does not ensure that those therapy services are available and in practice these too are disappearing along with personalisation and individual budgets.
Of course any client is free to fund their own mainstream recovery pathway and many do. The outcomes in this area alone (south-west London) have often been formidable. A composer who has funded her own recordings and launches now has self-employment through her music. Many are those who have accessed adult education courses and further training. Individuals have re-accessed faith venues which they had previously felt unable to enter for many years.
Not all these initiatives require direct payments - anyway those have now dried up. Many activities are free to access or funded by individual clients from their own pockets. Where direct payment has been needed it has often made the crucial difference.
Third-sector organisations also do great work in promoting access to mainstream through a variety of initiatives. 'Emergence' is an arts group run by and for service users who are also visual artists. In London and around the country 'Emergence' has pioneered access to visual arts as well as giving a platform for creativity and exhibition spaces for artists with personality disorder.
'Imagine' in south west London and Surrey also promotes a variety of arts opportunities including music production and visual arts. These are open to service users but take place in mainstream settings.
Mainstream environments have their own health, safety and insurance policies. As a consumer, the service user to entitled to the protection of these policies along with every other mainstream customer and client.
business,social inclusion
direct payments,
mainstream,
recovery
Wednesday 18 August 2010
Recovery & inclusion from NHS North West
Mental Health & Social Care Trust helps service users back into employment
Manchester Mental Health and Social Care Trust are committed to a recovery approach to mental health care. One element of this is to support service users who want to move into employment. They are currently piloting an Individual Placement and Support (IPS) service, funded by NHS North West.
The project consists of three Employment Specialists, based with Community Mental Health Teams, who help service users to find and remain in employment. The service offers help in preparing for work and engages with both employer and employee to provide ongoing support.
Joanne, one of the service users, is just one of the people to benefit from the pilot so far. After discussing her wish to get back into work with her Community Psychiatric Nurse (CPN) she was referred to the team's Employment Specialist who used the Mental Health Recovery star to talk through Joanne's situation and where she wanted to be in terms of finding a job. They then developed an action plan and the Employment Specialist helped Joanne to find jobs that were suited to her work history and aspirations. Joanne decided that working part time would be the best way to ease back into work life and through regular meetings, the Employment Specialist helped her to explore job vacancies. Eventually they identified one position that suited Joanne in terms of job description, location and number of hours.
The Employment Specialist arranged a meeting with the Disability Employment Adviser at the local Job Centre for support with in-work benefit calculations, and completing a permitted work form with a supporting letter from the Employment Specialist. 10 weeks after engaging with the IPS service, Joanne was successful at securing a Receptionist post for 12 hours a week and stays in touch with her Employment Specialist who provides in work support.
For more information please contact Zeph Curwen, Service Manager Occupational Activity & Employment, zeph.curwen@mhsc.nhs.uk or 0161 720 4809.
For more information on the IPS project contact Lucy Rowe in the Health and Work Programme, Workforce Directorate: lucy.rowe@northwest.nhs.uk or 0161 625 7350.
Manchester Mental Health and Social Care Trust are committed to a recovery approach to mental health care. One element of this is to support service users who want to move into employment. They are currently piloting an Individual Placement and Support (IPS) service, funded by NHS North West.
The project consists of three Employment Specialists, based with Community Mental Health Teams, who help service users to find and remain in employment. The service offers help in preparing for work and engages with both employer and employee to provide ongoing support.
Joanne, one of the service users, is just one of the people to benefit from the pilot so far. After discussing her wish to get back into work with her Community Psychiatric Nurse (CPN) she was referred to the team's Employment Specialist who used the Mental Health Recovery star to talk through Joanne's situation and where she wanted to be in terms of finding a job. They then developed an action plan and the Employment Specialist helped Joanne to find jobs that were suited to her work history and aspirations. Joanne decided that working part time would be the best way to ease back into work life and through regular meetings, the Employment Specialist helped her to explore job vacancies. Eventually they identified one position that suited Joanne in terms of job description, location and number of hours.
The Employment Specialist arranged a meeting with the Disability Employment Adviser at the local Job Centre for support with in-work benefit calculations, and completing a permitted work form with a supporting letter from the Employment Specialist. 10 weeks after engaging with the IPS service, Joanne was successful at securing a Receptionist post for 12 hours a week and stays in touch with her Employment Specialist who provides in work support.
For more information please contact Zeph Curwen, Service Manager Occupational Activity & Employment, zeph.curwen@mhsc.nhs.uk or 0161 720 4809.
For more information on the IPS project contact Lucy Rowe in the Health and Work Programme, Workforce Directorate: lucy.rowe@northwest.nhs.uk or 0161 625 7350.
Friday 30 July 2010
Derbyshire's personalisation champion
Personalisation, individual budgets, direct payments have all been around for some time. The particular significance for mental health and recovery is highlighted by some of the action that has been taken by service users.
Tony Martin has been speaking up for people with mental health problems since he started using services 15 years ago. In 2006 he took up a direct payment and became a convert to personalisation.
When the Department of Health started piloting individual budgets in 2005, he was appointed as a citizen leader tasked with promoting self-directed support.
Becoming a Mind personalisation champion was an extension of what he was doing already, though the cachet of saying he was working for Mind helped open more doors.
Martin aimed to increase the number of mental health service users with a direct payment in Derbyshire. As champion, he used his established links with the local primary care trust, the county council, government and with service users and service user forums.
He even held a conference on personal budgets to disseminate thinking. Attended by 140 people, including professionals, carers and service users, all groups felt they had learned a great deal.
Tackling professionals' attitudes and levels of knowledge about personalisation was key.
Martin says: "The real crux of it is ignorance in the service teams about how a direct payment can be used differently in mental health compared with in other groups, such as people with disabilities.
"It's no good thinking about how you can get people out of bed. It's about being able to give us new focuses and new interests in life and improving our quality of life."
Martin's analysis of 'ignorance in the service teams' is probably no longer as relevant as it was when he made the original comment. Mental health teams are very clued-in with the importance of direct payments as a potential route to mainstream above and beyond simple arrangements for care provision.
Service users like Martin and user groups are also pioneering creative uses for direct payments. Also, independent brokers working alongside mental health teams can help to ensure that direct payments and personalisation go hand-in-hand. Ultimately, personalisation can only exist for the sole purpose of enabling individuals' dreams, hopes and aspirations in the mainstream world.
Tony Martin's championing of direct payments for mental health led to a dramatic increase in take-up. By March 2010 there were 52 mental health service users with a direct payment in Derbyshire, up from 16 in September 2009, when Martin started his work as a champion.
Tony Martin has been speaking up for people with mental health problems since he started using services 15 years ago. In 2006 he took up a direct payment and became a convert to personalisation.
When the Department of Health started piloting individual budgets in 2005, he was appointed as a citizen leader tasked with promoting self-directed support.
Becoming a Mind personalisation champion was an extension of what he was doing already, though the cachet of saying he was working for Mind helped open more doors.
Martin aimed to increase the number of mental health service users with a direct payment in Derbyshire. As champion, he used his established links with the local primary care trust, the county council, government and with service users and service user forums.
He even held a conference on personal budgets to disseminate thinking. Attended by 140 people, including professionals, carers and service users, all groups felt they had learned a great deal.
Tackling professionals' attitudes and levels of knowledge about personalisation was key.
Martin says: "The real crux of it is ignorance in the service teams about how a direct payment can be used differently in mental health compared with in other groups, such as people with disabilities.
"It's no good thinking about how you can get people out of bed. It's about being able to give us new focuses and new interests in life and improving our quality of life."
Martin's analysis of 'ignorance in the service teams' is probably no longer as relevant as it was when he made the original comment. Mental health teams are very clued-in with the importance of direct payments as a potential route to mainstream above and beyond simple arrangements for care provision.
Service users like Martin and user groups are also pioneering creative uses for direct payments. Also, independent brokers working alongside mental health teams can help to ensure that direct payments and personalisation go hand-in-hand. Ultimately, personalisation can only exist for the sole purpose of enabling individuals' dreams, hopes and aspirations in the mainstream world.
Tony Martin's championing of direct payments for mental health led to a dramatic increase in take-up. By March 2010 there were 52 mental health service users with a direct payment in Derbyshire, up from 16 in September 2009, when Martin started his work as a champion.
business,social inclusion
direct payments,
dreams,
first aid,
goals,
hopes,
interventions,
personalisation,
tony martin
Tuesday 27 July 2010
Bridge Building for Mainstream
Bridge building for mainstream is now incorporated into the care pathway for people recovering from mental health conditions.
Community mental health teams, occupational therapies, psychiatrists are all aware of the value of mainstream bridge building. Many community mental health teams actively promote mainstream as part of their in-house practice with clients. Service-user led initiatives are also widely encouraged.
Where mental health teams may not always the time and resources to promote mainstream fully, there are many outside organisations working alongside the teams. The benefits of referral to an outside non-clinical team can be considerable.
Mental health teams can often discuss mainstream with clients in a clinical or home setting. An outside organisation has more time and capacity to draw clients out into mainstream settings where a conversation can begin. This may well be and should be - a conversation about the client's hopes, dreams, goals and aspirations.
One of the bridge builder's roles is to help facilitate this conversation. Another role is to be clued-in with what mainstream has to offer. For example, a bridge builder specialising in arts and culture needs to know what outlets there are both locally and further afield. A client who wishes to develop skills in music production should be introduced to the mainstream venue or venues where this opportunity takes place.
Community mental health teams, occupational therapies, psychiatrists are all aware of the value of mainstream bridge building. Many community mental health teams actively promote mainstream as part of their in-house practice with clients. Service-user led initiatives are also widely encouraged.
Where mental health teams may not always the time and resources to promote mainstream fully, there are many outside organisations working alongside the teams. The benefits of referral to an outside non-clinical team can be considerable.
Mental health teams can often discuss mainstream with clients in a clinical or home setting. An outside organisation has more time and capacity to draw clients out into mainstream settings where a conversation can begin. This may well be and should be - a conversation about the client's hopes, dreams, goals and aspirations.
One of the bridge builder's roles is to help facilitate this conversation. Another role is to be clued-in with what mainstream has to offer. For example, a bridge builder specialising in arts and culture needs to know what outlets there are both locally and further afield. A client who wishes to develop skills in music production should be introduced to the mainstream venue or venues where this opportunity takes place.
business,social inclusion
bridge builder,
bridge building for mainstream,
goals,
social inclusion
Sunday 25 July 2010
Mainstream - the Cascade Effect
As a social inclusion bridge builder I work with clients with severe and enduring mental health diagnoses. They are referred or they self-refer with the desire to access mainstream life domains.
Clients aspire to a variety of mainstream choices. It might be volunteering or befriending, it may be arts activities, it might be employment or running your own business. Client aspirations may include sports, faith, education, training or a selection from any or all of these.
Enabling individuals with a 'severe and enduring' background is not always a straightforward process although it certainly can be sometimes. A client can be introduced to a mainstream outlet and it can work for him or her almost immediately. Other clients may be unready for mainstream for a variety of reasons. They may suffer a relapse before accessing the mainstream environment. They may visualise mainstream as another form of day service or statutory support system, which it isn't.
Equally, clients can sometimes express a wish to access mainstream out of a misplaced fear that not accessing it might in some way affect their payments and benefits. It can be a long process before the value and rewards of mainstream are understood.
What is true is that clients who successfully access or re-access mainstream in turn become examples of mainstream's effectiveness. Signposting to mainstream as part of the mental health recovery pathway is undoubtedly effective, even if it does not work for everyone straight away.
Mainstream also helps to sustain recovery in the individual and even better, it can propagate more success and recovery out of its own resources. An example of this would be the musician who successfully links up with a mainstream recording studio. After months of regular rehearsal the musician is invited by the studio manager to contribute to a recording session. I witness this kind of beautiful outcome and its benefits for the client in my work as an arts bridge builder.
Another example - again from music bridge building - is the guitarist client who uses a studio regularly and invites a friend to join him during the session. The friend may well be another mental health service user who has never successfully engaged with mainstream despite the best efforts of the bridge building service. Where services have been unsuccessful a friendship and peer network can do the job far more effectively.
Mainstream reaches the places other services cannot reach and in the process it is able to create a cascade effect - a continuing path of development, recovery and individual growth.
Clients aspire to a variety of mainstream choices. It might be volunteering or befriending, it may be arts activities, it might be employment or running your own business. Client aspirations may include sports, faith, education, training or a selection from any or all of these.
Enabling individuals with a 'severe and enduring' background is not always a straightforward process although it certainly can be sometimes. A client can be introduced to a mainstream outlet and it can work for him or her almost immediately. Other clients may be unready for mainstream for a variety of reasons. They may suffer a relapse before accessing the mainstream environment. They may visualise mainstream as another form of day service or statutory support system, which it isn't.
Equally, clients can sometimes express a wish to access mainstream out of a misplaced fear that not accessing it might in some way affect their payments and benefits. It can be a long process before the value and rewards of mainstream are understood.
What is true is that clients who successfully access or re-access mainstream in turn become examples of mainstream's effectiveness. Signposting to mainstream as part of the mental health recovery pathway is undoubtedly effective, even if it does not work for everyone straight away.
Mainstream also helps to sustain recovery in the individual and even better, it can propagate more success and recovery out of its own resources. An example of this would be the musician who successfully links up with a mainstream recording studio. After months of regular rehearsal the musician is invited by the studio manager to contribute to a recording session. I witness this kind of beautiful outcome and its benefits for the client in my work as an arts bridge builder.
Another example - again from music bridge building - is the guitarist client who uses a studio regularly and invites a friend to join him during the session. The friend may well be another mental health service user who has never successfully engaged with mainstream despite the best efforts of the bridge building service. Where services have been unsuccessful a friendship and peer network can do the job far more effectively.
Mainstream reaches the places other services cannot reach and in the process it is able to create a cascade effect - a continuing path of development, recovery and individual growth.
business,social inclusion
arts,
growth,
mainstream,
music,
recording,
recovery,
self-development
Thursday 22 July 2010
Traditional cohorts
Service providers, staff, service users and carers are often perceived as the main groups comprising the traditional cohort of secondary mental health care provision. All this changes when mainstream practice is incorporated into care pathways. The effect of mainstreaming is that it introduces new stakeholders into the equation. Stakeholders chosen by the client as part of his or her recovery. Person-centred practice is designed to enable the person in recovery to access activities and outlets of their own choice in the mainstream environment. These outlets can be anywhere and everywhere, depending on the client's personal goals, hopes and aspirations.
Mainstream effectively destroys the stigma attached to recovery as it is longer attached to special settings, wherever this is the individual's preferred choice.
Mainstream effectively destroys the stigma attached to recovery as it is longer attached to special settings, wherever this is the individual's preferred choice.
Monday 19 July 2010
Thursday 15 July 2010
Discussing Mainstream
Bridge building for mainstream is now incorporated into the care pathway for people recovering from mental health conditions.
Community mental health teams, occupational therapies, psychiatrists are all aware of the value of mainstream bridge building. Many community mental health teams actively promote mainstream as part of their in-house practice with clients. Service-user led initiatives are also widely encouraged.
Where mental health teams may not always the time and resources to promote mainstream fully, there are many outside organisations working alongside the teams. The benefits of referral to an outside non-clinical team can be considerable.
Mental health teams can often discuss mainstream with clients in a clinical or home setting. An outside organisation has more time and capacity to draw clients out into mainstream settings where a conversation can begin. This may well be and should be - a conversation about the client's hopes, dreams, goals and aspirations.
One of the bridge builder's roles is to help facilitate this conversation. Another role is to be clued-in with what mainstream has to offer. For example, a bridge builder specialising in arts and culture needs to know what outlets there are both locally and further afield. A client who wishes to develop skills in music production should be introduced to the mainstream venue or venues where this opportunity takes place.
Community mental health teams, occupational therapies, psychiatrists are all aware of the value of mainstream bridge building. Many community mental health teams actively promote mainstream as part of their in-house practice with clients. Service-user led initiatives are also widely encouraged.
Where mental health teams may not always the time and resources to promote mainstream fully, there are many outside organisations working alongside the teams. The benefits of referral to an outside non-clinical team can be considerable.
Mental health teams can often discuss mainstream with clients in a clinical or home setting. An outside organisation has more time and capacity to draw clients out into mainstream settings where a conversation can begin. This may well be and should be - a conversation about the client's hopes, dreams, goals and aspirations.
One of the bridge builder's roles is to help facilitate this conversation. Another role is to be clued-in with what mainstream has to offer. For example, a bridge builder specialising in arts and culture needs to know what outlets there are both locally and further afield. A client who wishes to develop skills in music production should be introduced to the mainstream venue or venues where this opportunity takes place.
business,social inclusion
arts,
mainstream,
recording,
social inclusion,
studio
Linked Advertising
business,social inclusion
art,
buskers,
development,
london,
music,
songs,
songwriting
Wednesday 14 July 2010
Mainstream and the law
The Disability Discrimination Act (DDA 2005) makes it unlawful for a service provider to discriminate against a disabled person by refusing to provide any service which it provides to members of the public.”
'Service provider' refers to public and commercial sectors alike. A service provider may be a retail outlet, an NHS service, an employment bureau, a police station, a dating agency....the list is endless.
The implications for mainstream are highly significant. Clients referred from backgrounds of mental ill-health to mainstream life will encounter a new range of service providers. It is a social inclusion bridge builder's role to ensure that clients accessing mainstream are introduced to any service providers the client may have identified as key. Once a client is engaging with the services or products of that provider, he or she will be a beneficiary of the policies, procedures, insurance and legal obligations of that provider. The service user becomes equal with all the other consumers who are accessing mainstream as a matter of course. Consumers' rights are considerable.
Another result of the mainstream process is that it puts the responsibility for provision onto the mainstream provider. A client accessing a mainstream service such as a recording studio, for example, is a beneficiary of all that the studio provides. Provides not merely in terms of the studio service and products, but also in terms of the studio's policies, procedures, insurance and legal obligations. Equality with every other consumer creates an equal opportunities situation for the person now accessing mainstream.
Mainstream is not required to provide 'special settings' and nor should it. Mainstream should not stigmatize because of its awareness or unawareness of mental health issues. It should not stigmatize because stigma is not part of any reasonable access to a mainstream product or service.
'Service provider' refers to public and commercial sectors alike. A service provider may be a retail outlet, an NHS service, an employment bureau, a police station, a dating agency....the list is endless.
The implications for mainstream are highly significant. Clients referred from backgrounds of mental ill-health to mainstream life will encounter a new range of service providers. It is a social inclusion bridge builder's role to ensure that clients accessing mainstream are introduced to any service providers the client may have identified as key. Once a client is engaging with the services or products of that provider, he or she will be a beneficiary of the policies, procedures, insurance and legal obligations of that provider. The service user becomes equal with all the other consumers who are accessing mainstream as a matter of course. Consumers' rights are considerable.
Another result of the mainstream process is that it puts the responsibility for provision onto the mainstream provider. A client accessing a mainstream service such as a recording studio, for example, is a beneficiary of all that the studio provides. Provides not merely in terms of the studio service and products, but also in terms of the studio's policies, procedures, insurance and legal obligations. Equality with every other consumer creates an equal opportunities situation for the person now accessing mainstream.
Mainstream is not required to provide 'special settings' and nor should it. Mainstream should not stigmatize because of its awareness or unawareness of mental health issues. It should not stigmatize because stigma is not part of any reasonable access to a mainstream product or service.
business,social inclusion
access,
arts,
commercial,
dating agency,
mainstream,
mental health,
products,
recording,
retail,
services,
studio
Tuesday 13 July 2010
History of Social Inclusion
Social Inclusion and mainstream arise out of a history and out of a history of ideas.
Government think-tanks in the late 1990s and early 2000s had a key role in developing current thinking and practice around social inclusion. The envisaging of 'social domains' relevant to people's lives arises from these seminal ideas. The role of mainstream bridge builder is also developed around the concept of mainstream as a pathway for mental health recovery.
Social Inclusion goes back even further. A single act of defiance by Rosa Parks in 1955 in Alabama Mississippi. A black woman refusing to give up her seat on the bus to a white person, thereby defying the segregration laws. A key moment that lies at the heart of the civil rights movement, not just for the United States but for equality and social inclusion everywhere.
Equal opportunities, diversity, social inclusion and fairness are now commonplaces, enshrined in the way we strive to live and work today.
Government think-tanks in the late 1990s and early 2000s had a key role in developing current thinking and practice around social inclusion. The envisaging of 'social domains' relevant to people's lives arises from these seminal ideas. The role of mainstream bridge builder is also developed around the concept of mainstream as a pathway for mental health recovery.
Social Inclusion goes back even further. A single act of defiance by Rosa Parks in 1955 in Alabama Mississippi. A black woman refusing to give up her seat on the bus to a white person, thereby defying the segregration laws. A key moment that lies at the heart of the civil rights movement, not just for the United States but for equality and social inclusion everywhere.
Equal opportunities, diversity, social inclusion and fairness are now commonplaces, enshrined in the way we strive to live and work today.
business,social inclusion
business,
recovery,
Rosa Parks,
social inclusion
Monday 12 July 2010
Tools for Social Inclusion
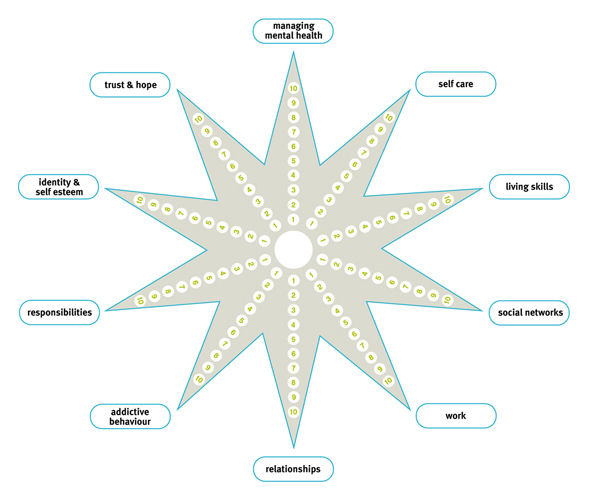
Two major assessment tools have been developed for social inclusion. One is the social inclusion 'Web' and the other is the 'Star' or 'Recovery Star'.
Originally created by the National Development Team (NDT) the web is a simple and effective assessment tool based on five key social domains. The domains were identified as key in the research done in the late 90s and early 2000s around social inclusion.
On the web these domains appear as:
Employment
Education & Training
Arts & Culture
Faith & Cultural Communities
Volunteering & Befriending
Family & Neighbourhood
Services
What makes the web unique for mental health is that it does not record or measure symptoms or diagnoses. A client who wishes to record which services he or she accesses may include the psychiatrist or community mental health team. However, the main purpose of the web is to record the client's involvement in mainstream. More importantly, the web is there to identify client's goals and aspirations in terms of where he or she wishes to be in mainstream.
Originally created by the National Development Team (NDT) the web is a simple and effective assessment tool based on five key social domains. The domains were identified as key in the research done in the late 90s and early 2000s around social inclusion.
On the web these domains appear as:
Employment
Education & Training
Arts & Culture
Faith & Cultural Communities
Volunteering & Befriending
Family & Neighbourhood
Services
What makes the web unique for mental health is that it does not record or measure symptoms or diagnoses. A client who wishes to record which services he or she accesses may include the psychiatrist or community mental health team. However, the main purpose of the web is to record the client's involvement in mainstream. More importantly, the web is there to identify client's goals and aspirations in terms of where he or she wishes to be in mainstream.
business,social inclusion
arts,
mainstream,
social inclusion,
star,
tools,
web
Sunday 11 July 2010
Social Inclusion - the mantra and the tantra
Social Inclusion - Does it exist?
Social Inclusion has long been a mantra for organisations representing clients who may be isolated or marginalised for one reason or another. Government think-tanks in the early 2000s identified key areas or social domains relevant to people's lives and development in the mainstream world. These are: employment, the arts, spirituality & cultural identity, volunteering, sports & healthy living, family and neighbourhood.
As a social inclusion bridge builder for mental health, I work with clients who wish to access Arts & Culture . The social inclusion approach will ask a client to identify which social domains they would like to prioritise for inclusion in mainstream. The bridge builder's role is then to signpost the client to the mainstream domain which has been prioritised. In order to facilitate this, bridge builders must have a wide network of local and regional contacts in his or her field of expertise. Further support relates only to how much or how little the client requests.
As Arts bridge builder for example, I need to know what is out there for clients who may wish to do arts courses or rehearse and record their music. Other clients may be seeking self-employment through tutoring, performing or composing. All of these aspirational goals have had successful outcomes, some of them quite outstanding. All the clients referred to mainstream come from a background of 'severe and enduring' mental health conditions.
The bridge building service is not a clinical or diagnostic one, although we work closely with Community Mental Health Teams. It is designed to enable clients to participate in mainstream, based on their own preferences, choices, skills and dreams. Clients are free to choose whether to disclose their illnesses or not.
When the arts bridge builder meets with a client, the key questions are 'what do you wish to see happen for yourself' or 'what would you like to do'. Bridge building focuses on aspiration, goals and innate gifts and talents. And that's it.
Social Inclusion has long been a mantra for organisations representing clients who may be isolated or marginalised for one reason or another. Government think-tanks in the early 2000s identified key areas or social domains relevant to people's lives and development in the mainstream world. These are: employment, the arts, spirituality & cultural identity, volunteering, sports & healthy living, family and neighbourhood.
As a social inclusion bridge builder for mental health, I work with clients who wish to access Arts & Culture . The social inclusion approach will ask a client to identify which social domains they would like to prioritise for inclusion in mainstream. The bridge builder's role is then to signpost the client to the mainstream domain which has been prioritised. In order to facilitate this, bridge builders must have a wide network of local and regional contacts in his or her field of expertise. Further support relates only to how much or how little the client requests.
As Arts bridge builder for example, I need to know what is out there for clients who may wish to do arts courses or rehearse and record their music. Other clients may be seeking self-employment through tutoring, performing or composing. All of these aspirational goals have had successful outcomes, some of them quite outstanding. All the clients referred to mainstream come from a background of 'severe and enduring' mental health conditions.
The bridge building service is not a clinical or diagnostic one, although we work closely with Community Mental Health Teams. It is designed to enable clients to participate in mainstream, based on their own preferences, choices, skills and dreams. Clients are free to choose whether to disclose their illnesses or not.
When the arts bridge builder meets with a client, the key questions are 'what do you wish to see happen for yourself' or 'what would you like to do'. Bridge building focuses on aspiration, goals and innate gifts and talents. And that's it.
business,social inclusion
arts,
mainstream,
social inclusion
How Social Inclusion is good for business
Social Inclusion - so good for business
The business case for mental health awareness is evidenced by the increasing numbers of employers who are commissioning mental health awareness trainings for their workforce. Employers want trainings which enable their staff to understand more about common mental health conditions. Understanding mental health means that staff can work better with clients and customers. It also allows staff to feel less isolated about personal issues around health and well-being.
Mental health awareness provides the opportunity for employers and employees to find out more about the law as it relates to employment and mental health.
Enlightened employers will seek to develop a workforce team which is happy rather than unhappy, fulfilled rather than excluded. Courses such as MHFA (Mental Health First Aid) show that attendees often feel that one of the benefits of the training in that it allows for a safe space. A safe space where individuals can share feelings about their personal well-being in addition to learning about the broader aspects of mental health conditions and the appropriate interventions.
In addition to mental health, it makes solid sense for businesses to incorporate awareness of social inclusion and mainstream. Returning to or accessing mainstream living is now a key part of the care pathway for those diagnosed with 'severe and enduring' mental health diagnoses. It is equally important for people who may be experiencing conditions such as anxiety, phobia or stress at work.
Both groups - those in primary and secondary care - are being signposted to mainstream life rather than to special settings as a central plank of the recovery process. The implications for any service provider - and that includes businesses - are crucial. Businesses and services are at the receiving end of mainstream.
Clients in recovery are choosing to access their personal goals through a diverse range of outlets. These could range from faith venues to volunteer bureaus, from retail outlets to sports centres, from recording studios to adult education colleges, from libraries to personal counselors, from training venues to department stores.
For businesses, it's not just one in four of their staff who may be experiencing mental health challenges, it's also one in four of their clients, customers and service consumers. Mental health challenges will also have an impact on one in three families. Disclosed or undisclosed, it's clear that mental health and well-being lie at the heart of our transactions and interactions.
The business case for mental health awareness is evidenced by the increasing numbers of employers who are commissioning mental health awareness trainings for their workforce. Employers want trainings which enable their staff to understand more about common mental health conditions. Understanding mental health means that staff can work better with clients and customers. It also allows staff to feel less isolated about personal issues around health and well-being.
Mental health awareness provides the opportunity for employers and employees to find out more about the law as it relates to employment and mental health.
Enlightened employers will seek to develop a workforce team which is happy rather than unhappy, fulfilled rather than excluded. Courses such as MHFA (Mental Health First Aid) show that attendees often feel that one of the benefits of the training in that it allows for a safe space. A safe space where individuals can share feelings about their personal well-being in addition to learning about the broader aspects of mental health conditions and the appropriate interventions.
In addition to mental health, it makes solid sense for businesses to incorporate awareness of social inclusion and mainstream. Returning to or accessing mainstream living is now a key part of the care pathway for those diagnosed with 'severe and enduring' mental health diagnoses. It is equally important for people who may be experiencing conditions such as anxiety, phobia or stress at work.
Both groups - those in primary and secondary care - are being signposted to mainstream life rather than to special settings as a central plank of the recovery process. The implications for any service provider - and that includes businesses - are crucial. Businesses and services are at the receiving end of mainstream.
Clients in recovery are choosing to access their personal goals through a diverse range of outlets. These could range from faith venues to volunteer bureaus, from retail outlets to sports centres, from recording studios to adult education colleges, from libraries to personal counselors, from training venues to department stores.
For businesses, it's not just one in four of their staff who may be experiencing mental health challenges, it's also one in four of their clients, customers and service consumers. Mental health challenges will also have an impact on one in three families. Disclosed or undisclosed, it's clear that mental health and well-being lie at the heart of our transactions and interactions.
Wednesday 7 July 2010
Is anti-stigma the new stigma?
Is anti-stigma the new stigma?
The 'Time to Change' campaign challenges stigma and discrimination against people with mental health conditions. For the next phase of the campaign Time to Change is helping groups and individuals organise activities which actively cooperate in challenging discriminatory attitudes and behaviours.
Time to Change advises that 'at Get Moving events it is ideal if there is a 50/50 mix of individuals with experience of mental health problems and those without in order to maximise the amount of stigma broken down and the number of stereotypes challenged.' Events suggested are football games, group walks or 'a dance routine which is then performed'.
The campaign promotes 'social contact' and 'social contact theory' put into practice' to challenge stigma and discrimination'.
Why should people with mental health conditions have to access mainstream activities as part of a campaign?
Challenging discrimination is achieved primarily through engaging in mainstream as a contributor, a consumer or a provider. Many people with mental health conditions access mainstream activities, making their own choices as to whether to disclose or not. The most impact in challenging mainstream can be achieved by prioritising individual goals and aspirations. Support is also available to access mainstream from mental health organisations and bridge builders or through direct payments.
People who play football who happen to have mental health conditions are footballers. They aren't required to be 'positive mental health footballers'. People who play guitar who happen to have mental health conditions are guitarists, not mental health guitarists. People who are arts tutors who have a mental health condition are arts tutors. By continuing to tag mental health on mainstream activities and aspirations there is a danger of recycling stigma and not allowing people to move into valued social roles.
Could anti-stigma be the new stigma?
The 'Time to Change' campaign challenges stigma and discrimination against people with mental health conditions. For the next phase of the campaign Time to Change is helping groups and individuals organise activities which actively cooperate in challenging discriminatory attitudes and behaviours.
Time to Change advises that 'at Get Moving events it is ideal if there is a 50/50 mix of individuals with experience of mental health problems and those without in order to maximise the amount of stigma broken down and the number of stereotypes challenged.' Events suggested are football games, group walks or 'a dance routine which is then performed'.
The campaign promotes 'social contact' and 'social contact theory' put into practice' to challenge stigma and discrimination'.
Why should people with mental health conditions have to access mainstream activities as part of a campaign?
Challenging discrimination is achieved primarily through engaging in mainstream as a contributor, a consumer or a provider. Many people with mental health conditions access mainstream activities, making their own choices as to whether to disclose or not. The most impact in challenging mainstream can be achieved by prioritising individual goals and aspirations. Support is also available to access mainstream from mental health organisations and bridge builders or through direct payments.
People who play football who happen to have mental health conditions are footballers. They aren't required to be 'positive mental health footballers'. People who play guitar who happen to have mental health conditions are guitarists, not mental health guitarists. People who are arts tutors who have a mental health condition are arts tutors. By continuing to tag mental health on mainstream activities and aspirations there is a danger of recycling stigma and not allowing people to move into valued social roles.
Could anti-stigma be the new stigma?
business,social inclusion
arts,
inclusion,
mainstream,
social inclusion,
stigma
Sunday 4 July 2010
Saturday 3 July 2010
'Taking Care of Business' - Mind campaign
Mind’s ‘Taking care of Business’ campaign highlights the initiatives being taken by many employers around issues of mental health at work.
Supported by business ‘dragon’ Duncan Bannatyne, the campaign shows that employers are becoming aware of the need to address and support good mental health in the workplace.
The Mind campaign underlines the message that the promotion of good mental health helps employers ‘increase productivity, improve staff performance and save thousands of pounds’.
Mind also hosts a series of follow-up programmes designed to actively encourage good mental health in the workplace.
Some of the companies who have signed up to support the Mind campaign include EDF energy, BT, Hewitt Consultancy, AXA and police and security services. James Kenrick at Hewitt Associates helped set up an Employee Assistance programme allowing staff access to counselling services where appropriate.
Hewitt also initiated a staff health audit which identified stress, anxiety and depression as ‘real issues within the organisation’. James Kenrick states that:
‘after the health audit we sourced a stress vocational rehabilitation service, which has a vocational focus and is staffed by psychologists. Employees who have been absent for 10 days or more are referred for an initial assessment, and recommended the most appropriate treatment plan. We have found that this service, along with early intervention, has greatly reduced the days lost through stress-related absence and stopped stress-related disability altogether’.
Proactive management of mental health in the workplace has allowed Hewitt Associates to save ‘nearly £400’ per employee. More importantly, as Kenrick states:
‘it's the intangible elements that are most rewarding. The feedback from staff who have been helped to recover from difficult circumstances has been exceptional’.
EDF Energy is a major electricity provider. A workplace audit showed that the company was losing around £1.4m in productivity each year as a result of mental ill health among its employees. As part of an Employee Support Programme the company offered psychological support (cognitive behavioural therapy) to employees and trained over 1,000 managers to recognise psychological ill health among staff and to minimise its effects. This resulted in an improvement in productivity which saved the organisation approximately £228,000 per year. Job satisfaction also rose from 36 to 68% (Business in the Community, 2009).
Supported by business ‘dragon’ Duncan Bannatyne, the campaign shows that employers are becoming aware of the need to address and support good mental health in the workplace.
The Mind campaign underlines the message that the promotion of good mental health helps employers ‘increase productivity, improve staff performance and save thousands of pounds’.
Mind also hosts a series of follow-up programmes designed to actively encourage good mental health in the workplace.
Some of the companies who have signed up to support the Mind campaign include EDF energy, BT, Hewitt Consultancy, AXA and police and security services. James Kenrick at Hewitt Associates helped set up an Employee Assistance programme allowing staff access to counselling services where appropriate.
Hewitt also initiated a staff health audit which identified stress, anxiety and depression as ‘real issues within the organisation’. James Kenrick states that:
‘after the health audit we sourced a stress vocational rehabilitation service, which has a vocational focus and is staffed by psychologists. Employees who have been absent for 10 days or more are referred for an initial assessment, and recommended the most appropriate treatment plan. We have found that this service, along with early intervention, has greatly reduced the days lost through stress-related absence and stopped stress-related disability altogether’.
Proactive management of mental health in the workplace has allowed Hewitt Associates to save ‘nearly £400’ per employee. More importantly, as Kenrick states:
‘it's the intangible elements that are most rewarding. The feedback from staff who have been helped to recover from difficult circumstances has been exceptional’.
EDF Energy is a major electricity provider. A workplace audit showed that the company was losing around £1.4m in productivity each year as a result of mental ill health among its employees. As part of an Employee Support Programme the company offered psychological support (cognitive behavioural therapy) to employees and trained over 1,000 managers to recognise psychological ill health among staff and to minimise its effects. This resulted in an improvement in productivity which saved the organisation approximately £228,000 per year. Job satisfaction also rose from 36 to 68% (Business in the Community, 2009).
business,social inclusion
business,
duncan bannatyne,
mind,
social inclusionusiness
Monday 21 June 2010
Friday 18 June 2010
Freeindex Profile
If you have attended a recent training, please feel free to review me.
Freeindex listing:
Freeindex listing:
Monday 14 June 2010
Traditional cohorts in care provision
Service providers, staff, service users and carers are often perceived as the main groups comprising the traditional cohort of secondary mental health care provision. All this changes when mainstream practice is incorporated into care pathways. The effect of mainstreaming is that it introduces new stakeholders into the equation. Stakeholders chosen by the client as part of his or her recovery. Person-centred practice is designed to enable the person in recovery to access activities and outlets of their own choice in the mainstream environment. These outlets can be anywhere and everywhere, depending on the client's personal goals, hopes and aspirations.
Mainstream effectively destroys the stigma attached to recovery as it is longer attached to special settings, wherever this is the individual's preferred choice.
Mainstream effectively destroys the stigma attached to recovery as it is longer attached to special settings, wherever this is the individual's preferred choice.
Tuesday 8 June 2010
'Taking Care of Business' - Mind campaign
Mind’s ‘Taking care of Business’ campaign highlights the initiatives being taken by many employers around issues of mental health at work.
Supported by business ‘dragon’ Duncan Bannatyne, the campaign shows that employers are becoming aware of the need to address and support good mental health in the workplace.
The Mind campaign underlines the message that the promotion of good mental health helps employers ‘increase productivity, improve staff performance and save thousands of pounds’.
Mind also hosts a series of follow-up programmes designed to actively encourage good mental health in the workplace.
Some of the companies who have signed up to support the Mind campaign include EDF energy, BT, Hewitt Consultancy, AXA and police and security services. James Kenrick at Hewitt Associates helped set up an Employee Assistance programme allowing staff access to counselling services where appropriate.
Hewitt also initiated a staff health audit which identified stress, anxiety and depression as ‘real issues within the organisation’. James Kenrick states that:
‘after the health audit we sourced a stress vocational rehabilitation service, which has a vocational focus and is staffed by psychologists. Employees who have been absent for 10 days or more are referred for an initial assessment, and recommended the most appropriate treatment plan. We have found that this service, along with early intervention, has greatly reduced the days lost through stress-related absence and stopped stress-related disability altogether’.
Proactive management of mental health in the workplace has allowed Hewitt Associates to save ‘nearly £400’ per employee. More importantly, as Kenrick states:
‘it's the intangible elements that are most rewarding. The feedback from staff who have been helped to recover from difficult circumstances has been exceptional’.
EDF Energy is a major electricity provider. A workplace audit showed that the company was losing around £1.4m in productivity each year as a result of mental ill health among its employees. As part of an Employee Support Programme the company offered psychological support (cognitive behavioural therapy) to employees and trained over 1,000 managers to recognise psychological ill health among staff and to minimise its effects. This resulted in an improvement in productivity which saved the organisation approximately £228,000 per year. Job satisfaction also rose from 36 to 68% (Business in the Community, 2009).
Supported by business ‘dragon’ Duncan Bannatyne, the campaign shows that employers are becoming aware of the need to address and support good mental health in the workplace.
The Mind campaign underlines the message that the promotion of good mental health helps employers ‘increase productivity, improve staff performance and save thousands of pounds’.
Mind also hosts a series of follow-up programmes designed to actively encourage good mental health in the workplace.
Some of the companies who have signed up to support the Mind campaign include EDF energy, BT, Hewitt Consultancy, AXA and police and security services. James Kenrick at Hewitt Associates helped set up an Employee Assistance programme allowing staff access to counselling services where appropriate.
Hewitt also initiated a staff health audit which identified stress, anxiety and depression as ‘real issues within the organisation’. James Kenrick states that:
‘after the health audit we sourced a stress vocational rehabilitation service, which has a vocational focus and is staffed by psychologists. Employees who have been absent for 10 days or more are referred for an initial assessment, and recommended the most appropriate treatment plan. We have found that this service, along with early intervention, has greatly reduced the days lost through stress-related absence and stopped stress-related disability altogether’.
Proactive management of mental health in the workplace has allowed Hewitt Associates to save ‘nearly £400’ per employee. More importantly, as Kenrick states:
‘it's the intangible elements that are most rewarding. The feedback from staff who have been helped to recover from difficult circumstances has been exceptional’.
EDF Energy is a major electricity provider. A workplace audit showed that the company was losing around £1.4m in productivity each year as a result of mental ill health among its employees. As part of an Employee Support Programme the company offered psychological support (cognitive behavioural therapy) to employees and trained over 1,000 managers to recognise psychological ill health among staff and to minimise its effects. This resulted in an improvement in productivity which saved the organisation approximately £228,000 per year. Job satisfaction also rose from 36 to 68% (Business in the Community, 2009).
Wednesday 2 June 2010
Sunday 30 May 2010
The Business Case for Mental Health Awareness
The economic and social cost of mental health problems in the United Kingdom is well documented. In 2002/03 the economic and social cost of mental health problems in England was £77 billion. (SCMH, 2003). The economic and social cost of mental health problems is greater than that of crime and larger than the total amount spent on all NHS and social services in the UK (HM Treasury, 2005).
Dame Carol Black's 2008 report 'Working for a Healthier Tomorrow' was a major attempt to address these concerns. Legislative review such as the 2005 amendments to the Disability Discrimination Act (DDA) highlighted the need to address the massive economic and social attrition behind issues of mental ill-health. In 2005 the Confederation of British Industry was concerned enough to commission its own research. Stress, anxiety and depression accounted for a third of the 168 million working days lost in the UK for health and related reasons in 2004, translating to a cost of sickness absence of about £4.1 billion (Confederation of British Industry, 2005).
As a result of legislation, employees have more rights and employers more responsibilities relating to the incidence of mental health in the workplace. Employees who choose to disclose a mental health condition to their employers are strongly protected by legislation and have the right to 'reasonable adjustments' that they may request their employers to make. In practice, it is still true that people with mental health diagnoses may well feel little confidence in this legislation. Nonetheless, their rights are enshrined in law. Similarly, employers have a legal responsibility not to discriminate against employees who have disclosed a mental health condition and to make any reasonable adjustments that have been requested.
Dame Carol Black's 2008 report 'Working for a Healthier Tomorrow' was a major attempt to address these concerns. Legislative review such as the 2005 amendments to the Disability Discrimination Act (DDA) highlighted the need to address the massive economic and social attrition behind issues of mental ill-health. In 2005 the Confederation of British Industry was concerned enough to commission its own research. Stress, anxiety and depression accounted for a third of the 168 million working days lost in the UK for health and related reasons in 2004, translating to a cost of sickness absence of about £4.1 billion (Confederation of British Industry, 2005).
As a result of legislation, employees have more rights and employers more responsibilities relating to the incidence of mental health in the workplace. Employees who choose to disclose a mental health condition to their employers are strongly protected by legislation and have the right to 'reasonable adjustments' that they may request their employers to make. In practice, it is still true that people with mental health diagnoses may well feel little confidence in this legislation. Nonetheless, their rights are enshrined in law. Similarly, employers have a legal responsibility not to discriminate against employees who have disclosed a mental health condition and to make any reasonable adjustments that have been requested.
business,social inclusion
carol black,
disability discrimination,
economy,
mental health
Friday 21 May 2010
Recovery
Recovery
Recovery is a process of hope and aspiration that signals the return to mainstream life for those who have experienced mental health problems. Recovery can take place regardless of whether the individual is symptom-free or not. Hope and recovery are recognised as key parts of the care pathway. Social inclusion bridge builders work with clients on a recovery programme based on the client's own choices and aspirations.
More about Recovery and the work of Dr. Pat Deegan
Recovery is a process of hope and aspiration that signals the return to mainstream life for those who have experienced mental health problems. Recovery can take place regardless of whether the individual is symptom-free or not. Hope and recovery are recognised as key parts of the care pathway. Social inclusion bridge builders work with clients on a recovery programme based on the client's own choices and aspirations.
More about Recovery and the work of Dr. Pat Deegan
business,social inclusion
aspiration,
inclusion,
pat deegan,
recovery
Thursday 20 May 2010
Planning for Good Mental Health & Social Inclusion: Course Testimonials
Planning for Good Mental Health & Social Inclusion
Training testimonials:
'Such a huge subject - well covered in the time allotted'.
'The course has enabled me to be 'more assertive in recognising and prioritising mental health issues'.
I shall 'develop a knowledge base of local services and encourage others to make appropriate referrals'.
'John is a very calm person. Used the background music to create a non-threatening, relaxed atmosphere'.
I shall 'explore in greater depths what services are available to individual clients'.
'I feel I am more aware of what to look for in myself and others'.
The course 'has made me more aware of the need to ensure people return to mainstream after illness'.
'Ideas and information given to think outside the box'.
The course reinforced 'the importance of mainstream social inclusion'.
I now have 'more awareness of organisations and can utilise the social inclusion 'web' tool in assessments.'
Training testimonials:
'Such a huge subject - well covered in the time allotted'.
'The course has enabled me to be 'more assertive in recognising and prioritising mental health issues'.
I shall 'develop a knowledge base of local services and encourage others to make appropriate referrals'.
'John is a very calm person. Used the background music to create a non-threatening, relaxed atmosphere'.
I shall 'explore in greater depths what services are available to individual clients'.
'I feel I am more aware of what to look for in myself and others'.
The course 'has made me more aware of the need to ensure people return to mainstream after illness'.
'Ideas and information given to think outside the box'.
The course reinforced 'the importance of mainstream social inclusion'.
I now have 'more awareness of organisations and can utilise the social inclusion 'web' tool in assessments.'
business,social inclusion
mainstream,
planning for good mental health,
social inclusion
Planning for Good Mental Health & Social Inclusion
Planning for Good Mental Health & Social Inclusion
Commissioned by a major Surrey NHS Trust success the training 'Planning for Good Mental Health & Social Inclusion' has been a great success and is now running throughout 2010. Attendees include health visitors, GPs, occupational therapists, members, social workers and day centre workers. Library managers and staff have joined the training cohort, making for diverse and lively learning. The training has been put together by John Vanek, an experienced Social Inclusion bridge builder and qualified Mental Health First Aid Instructor.
Current attendees on the 'Planning for Good Mental Health & Social Inclusion' course cover a broad range of professional disciplines from across NHS and commissioning services. These have included Health Visitors, Social Workers, a service commissioner, a GP, specialised Physiotherapist and a Dietician.
The course is designed to be of benefit for anyone who is a service provider, not specifically within the caring or health professions.
Typical groups who benefit from the trainings include:
NHS and Primary Care Team staff evaluations for 'Planning for Good Mental Health & Social Inclusion' trainings.
Commissioned by a major Surrey NHS Trust success the training 'Planning for Good Mental Health & Social Inclusion' has been a great success and is now running throughout 2010. Attendees include health visitors, GPs, occupational therapists, members, social workers and day centre workers. Library managers and staff have joined the training cohort, making for diverse and lively learning. The training has been put together by John Vanek, an experienced Social Inclusion bridge builder and qualified Mental Health First Aid Instructor.
Current attendees on the 'Planning for Good Mental Health & Social Inclusion' course cover a broad range of professional disciplines from across NHS and commissioning services. These have included Health Visitors, Social Workers, a service commissioner, a GP, specialised Physiotherapist and a Dietician.
The course is designed to be of benefit for anyone who is a service provider, not specifically within the caring or health professions.
Typical groups who benefit from the trainings include:
- Employers who wish to know more about common mental health conditions
- Business owners who wish to address problems of lost productivity due to undiagnosed or diagnosed staff mental health problems
- Anyone who wishes to know more about current mental health legislation and their legal rights and requirements.
- Community-based workers who wish to learn about developments in social inclusion over the last fifty years.
- HR practitioners who wish to gain simple assessment skills and tools for helping clients or employees make a successful return to mainstream life after illness or setback.
- Health & Safety personnel keen to know more about what's out there for people who may be experiencing mild or more severe mental health challenges.
NHS and Primary Care Team staff evaluations for 'Planning for Good Mental Health & Social Inclusion' trainings.
business,social inclusion
planning for good mental health,
trainings
Wednesday 19 May 2010
Monday 17 May 2010
How mental health can enrich the work environment
People with mental health conditions who are returning to employment or even accessing it for the first time can often make exceptional contributions to the workplace.
Their previous experience can be considerable and many individuals returning to mainstream carry high levels of skills and expertise. It may also be the case that the previous workplace was a contributory factor and there is no desire to return to 'the scene of the crime'.
Individuals returning to mainstream often do so with care and caution. The pathway back to employment may begin with voluntary work or a part-time position. Often it provides an opportunity to discover an area of interest the individual has always wanted to take up but never had the chance. A part-time post in a related field can help to prepare the way for a full-time salaried position. The returning employee makes his or her way back into the workplace with new skills, new experiences and new life encounters.
An art tutor who understands mental illness from first-hand experience will apply non-discriminatory and more inclusive practice alongside his or her skills. An individual in recovery might discover through accessing a mainstream service that he or she has gifts that can be developed and extended.
The way back into mainstream for people who may have never worked due to illness needs to happen through gradual re-skilling and training. With good bridge building, clients can identify the kind of special gifts they may have never identified previously. Person-centred planning is designed to help clients discover genuine aspirations and goals. It is not designed to force individuals to fit into a particular job role nor to be assigned to sheltered employment outside mainstream, except where the individual feels this may be appropriate.
Identifying a suppressed aspiration as the cause of stress at work can lead to formidable achievement when previously hidden dreams are pursued and developed in the appropriate mainstream setting. This too creates employment or self-employment alongside increased cashflow and profits for the service providers and employers who are helping individual dreams to become reality.
Their previous experience can be considerable and many individuals returning to mainstream carry high levels of skills and expertise. It may also be the case that the previous workplace was a contributory factor and there is no desire to return to 'the scene of the crime'.
Individuals returning to mainstream often do so with care and caution. The pathway back to employment may begin with voluntary work or a part-time position. Often it provides an opportunity to discover an area of interest the individual has always wanted to take up but never had the chance. A part-time post in a related field can help to prepare the way for a full-time salaried position. The returning employee makes his or her way back into the workplace with new skills, new experiences and new life encounters.
An art tutor who understands mental illness from first-hand experience will apply non-discriminatory and more inclusive practice alongside his or her skills. An individual in recovery might discover through accessing a mainstream service that he or she has gifts that can be developed and extended.
The way back into mainstream for people who may have never worked due to illness needs to happen through gradual re-skilling and training. With good bridge building, clients can identify the kind of special gifts they may have never identified previously. Person-centred planning is designed to help clients discover genuine aspirations and goals. It is not designed to force individuals to fit into a particular job role nor to be assigned to sheltered employment outside mainstream, except where the individual feels this may be appropriate.
Identifying a suppressed aspiration as the cause of stress at work can lead to formidable achievement when previously hidden dreams are pursued and developed in the appropriate mainstream setting. This too creates employment or self-employment alongside increased cashflow and profits for the service providers and employers who are helping individual dreams to become reality.
business,social inclusion
art,
employment,
gifts,
mainstream,
skills
Wednesday 12 May 2010
Who should take an MHFA England course?
Who should take an MHFA England course?
Anyone can benefit from Mental Health First Aid (MHFA). It is open to members of the general public. Families affected by mental health problems, teachers, health service providers, emergency workers, frontline workers who deal with the public, volunteers, human resources professionals, employers and community groups are just a few of the groups who have benefited from MHFA.
Mental Health First Aid covers a comprehensive range of common mental health conditions and their appropriate first aid interventions. The conditions covered range from psychosis to phobia, from bi-polar to anxiety, from schizophrenia to stress at work. From this point-of-view MHFA is highly intensive, detailed and excellently put together.
It is important to bear in mind that MHFA is more than mental health awareness. A good mental health awareness course may well be a good 'Level I' for those who wish to find out more about general mental health before deciding to go on to MHFA at 'Level II'.
Anyone can benefit from Mental Health First Aid (MHFA). It is open to members of the general public. Families affected by mental health problems, teachers, health service providers, emergency workers, frontline workers who deal with the public, volunteers, human resources professionals, employers and community groups are just a few of the groups who have benefited from MHFA.
Mental Health First Aid covers a comprehensive range of common mental health conditions and their appropriate first aid interventions. The conditions covered range from psychosis to phobia, from bi-polar to anxiety, from schizophrenia to stress at work. From this point-of-view MHFA is highly intensive, detailed and excellently put together.
It is important to bear in mind that MHFA is more than mental health awareness. A good mental health awareness course may well be a good 'Level I' for those who wish to find out more about general mental health before deciding to go on to MHFA at 'Level II'.
Social Inclusion Facebook Group
Social Inclusion Facebook Group is now open for anyone interested in issues of social inclusion, health, mental health, arts, goals and dreams. Welcome!
Sunday 9 May 2010
The Business Case for Mental Health Awareness
The Business Case for Mental Health Awareness. The economic and social cost of mental health problems in the United Kingdom is well documented. In 2002/03 the economic and social cost of mental health problems in England was £77 billion. (SCMH, 2003). The economic and social cost of mental health problems is greater than that of crime and larger than the total amount spent on all NHS and social services in the UK (HM Treasury, 2005).
Dame Carol Black's 2008 report 'Working for a Healthier Tomorrow' was a major attempt to address these concerns. Legislative review such as the 2005 amendments to the Disability Discrimination Act (DDA) highlighted the need to address the massive economic and social attrition behind issues of mental ill-health. In 2005 the Confederation of British Industry was concerned enough to commission its own research. Stress, anxiety and depression accounted for a third of the 168 million working days lost in the UK for health and related reasons in 2004, translating to a cost of sickness absence of about £4.1 billion (Confederation of British Industry, 2005).
As a result of legislation, employees have more rights and employers more responsibilities relating to the incidence of mental health in the workplace. Employees who choose to disclose a mental health condition to their employers are strongly protected by legislation and have the right to 'reasonable adjustments' that they may request their employers to make. In practice, it is still true that people with mental health diagnoses may well feel little confidence in this legislation. Nonetheless, their rights are enshrined in law. Similarly, employers have a legal responsibility not to discriminate against employees who have disclosed a mental health condition and to make any reasonable adjustments that have been requested.
Dame Carol Black's 2008 report 'Working for a Healthier Tomorrow' was a major attempt to address these concerns. Legislative review such as the 2005 amendments to the Disability Discrimination Act (DDA) highlighted the need to address the massive economic and social attrition behind issues of mental ill-health. In 2005 the Confederation of British Industry was concerned enough to commission its own research. Stress, anxiety and depression accounted for a third of the 168 million working days lost in the UK for health and related reasons in 2004, translating to a cost of sickness absence of about £4.1 billion (Confederation of British Industry, 2005).
As a result of legislation, employees have more rights and employers more responsibilities relating to the incidence of mental health in the workplace. Employees who choose to disclose a mental health condition to their employers are strongly protected by legislation and have the right to 'reasonable adjustments' that they may request their employers to make. In practice, it is still true that people with mental health diagnoses may well feel little confidence in this legislation. Nonetheless, their rights are enshrined in law. Similarly, employers have a legal responsibility not to discriminate against employees who have disclosed a mental health condition and to make any reasonable adjustments that have been requested.
How businesses profit from mental health
How businesses profits from mental health.
Businesses and services are developing the understanding that informed practice around mental health benefits both service delivery and profits. Staff are happier and more productive when they know that their employers' practices and procedures do not stigmatize or discriminate against illness or experience.
Days lost to absenteeism, sickness or unproductive presenteeism decrease when employees are not anxious about being dismissed should they choose to disclose a mental health condition. The attrition of unexplained job resignations or sudden departures decreases when taboos around mental health are dismantled by enlightened policies and staff trainings.
Business and services profit from individuals who are being signposted to mainstream as part of their recovery plans. Mainstream social inclusion takes place in any outlet where a recovering individual feels he or she can prioritise a personal goal. Venues such as education and training centres, sports facilities, colleges, recording studios, voluntary organisations and arts groups are benefiting substantially and financially from motivated people accessing mainstream. Where individuals are not paying all the costs themselves, there may well be contributions from schemes such as direct payments or from built-in concessions and offers. The increased business generated by mainstream social inclusion is considerable.
Businesses and services are developing the understanding that informed practice around mental health benefits both service delivery and profits. Staff are happier and more productive when they know that their employers' practices and procedures do not stigmatize or discriminate against illness or experience.
Days lost to absenteeism, sickness or unproductive presenteeism decrease when employees are not anxious about being dismissed should they choose to disclose a mental health condition. The attrition of unexplained job resignations or sudden departures decreases when taboos around mental health are dismantled by enlightened policies and staff trainings.
Business and services profit from individuals who are being signposted to mainstream as part of their recovery plans. Mainstream social inclusion takes place in any outlet where a recovering individual feels he or she can prioritise a personal goal. Venues such as education and training centres, sports facilities, colleges, recording studios, voluntary organisations and arts groups are benefiting substantially and financially from motivated people accessing mainstream. Where individuals are not paying all the costs themselves, there may well be contributions from schemes such as direct payments or from built-in concessions and offers. The increased business generated by mainstream social inclusion is considerable.
business,social inclusion
business,
mental health,
social inclusion
Subscribe to:
Posts (Atom)