An ongoing series of articles on themes of social inclusion. More details of John's work and training schedules can be found at www.mhfatrainings.com MHFA England is the national licensed organisation for MHFA UK (www.mhfaengland.org.uk)
Showing posts with label recovery. Show all posts
Showing posts with label recovery. Show all posts
Monday, 23 July 2012
Friday, 10 June 2011
The bridge builder's role
Bridge building is a strategy developed in the late 1990s and early 2000s. Designed to promote social inclusion for groups that might otherwise be marginalised, bridge building has been used to immense effect in the mental health field. Bridge building is particularly useful for people who suffer or who are in recovery from severe and enduring mental health conditions.
The role of the bridge builder is very simple. It is to help facilitate access to mainstream environments for individuals, based entirely on their own personal choices. The original social inclusion think-tanks were set up by the (then) office of the deputy prime minister. Nine key social domains were identified as key to individual development. However, it is not expected that every individual would be expected to access every single domain, nor would they wish to. The key areas include employment, arts & culture, faith and cultural communities, education & training, volunteering, befriending, sports and wellbeing. There are other domains as well, such as friends and family and statutory services.
Within these contexts, a bridge building team can be set up, working in mainstream with referrals from other agencies particularly NHS and social services. It is crucial that the organisation that is commissioned to carry out mainstream is itself embedded in a mainstream environment or conducts its interactions with clients in the big wide world, rather than in a clinical setting. It is the only way that a conversation with a client about their hopes and aspirations can be realistic and genuine. These approaches are entirely in line with the way mainstream was envisaged as a key part of the care pathway and an alternative to what Dr. Pat Deegan has aptly described as 'a career in mental health'.
The role of the bridge builder is very simple. It is to help facilitate access to mainstream environments for individuals, based entirely on their own personal choices. The original social inclusion think-tanks were set up by the (then) office of the deputy prime minister. Nine key social domains were identified as key to individual development. However, it is not expected that every individual would be expected to access every single domain, nor would they wish to. The key areas include employment, arts & culture, faith and cultural communities, education & training, volunteering, befriending, sports and wellbeing. There are other domains as well, such as friends and family and statutory services.
Within these contexts, a bridge building team can be set up, working in mainstream with referrals from other agencies particularly NHS and social services. It is crucial that the organisation that is commissioned to carry out mainstream is itself embedded in a mainstream environment or conducts its interactions with clients in the big wide world, rather than in a clinical setting. It is the only way that a conversation with a client about their hopes and aspirations can be realistic and genuine. These approaches are entirely in line with the way mainstream was envisaged as a key part of the care pathway and an alternative to what Dr. Pat Deegan has aptly described as 'a career in mental health'.
business,social inclusion
art,
bridge builder,
pat deegan,
recovery
Friday, 18 March 2011
Clinical and social models of care in mental health
In the mental health field, it has long been accepted that clinical and social models of care go hand-in-hand. Doing more than simply addressing clinical symptoms is a requirement of the care pathway.
People who have experienced severe and enduring mental health conditions currently have access to a spectrum of professional care. This can range from the psychiatrist, the community mental health nurse, assertive outreach and social workers, O.T.s and other key personnel. Any or all of these individuals can currently form part of the care plan for people recovering from severe mental health conditions. In addition, there is access to third-party groups providing bridge building or similar services. The return to mainstream life based on individual choices forms a strong part of the clinical and social models working together.
So what will be the scenario when mental health moves into the sphere of general practice, along with a host of other clinical services?
In the UK, GP consortia are being set up with the intention of taking over from the primary care teams entirely by the year 2013. The primary care teams that currently incorporate a spectrum of care services for mental health will no longer exist. It is uncertain whether GP consortia and GP surgeries will be equipped to respond to providing the clinical and social models which currently operate. What this means is that there could be no access to the key services that are well-positioned to provide access for the individual to his or her independence, recovery and self-development.
The providers who currently enable access to mainstream life for people with mental health conditions will need to introduce themselves to the GP consortia as a matter of urgency. In order to become better placed to continue the work of mainstream recovery it will be important to do this now. Commercial and private providers are already muscling in on the GP consortia and it is unlikely that these groups will have any expertise at all in providing hope and aspiration for marginalised people.
People who have experienced severe and enduring mental health conditions currently have access to a spectrum of professional care. This can range from the psychiatrist, the community mental health nurse, assertive outreach and social workers, O.T.s and other key personnel. Any or all of these individuals can currently form part of the care plan for people recovering from severe mental health conditions. In addition, there is access to third-party groups providing bridge building or similar services. The return to mainstream life based on individual choices forms a strong part of the clinical and social models working together.
So what will be the scenario when mental health moves into the sphere of general practice, along with a host of other clinical services?
In the UK, GP consortia are being set up with the intention of taking over from the primary care teams entirely by the year 2013. The primary care teams that currently incorporate a spectrum of care services for mental health will no longer exist. It is uncertain whether GP consortia and GP surgeries will be equipped to respond to providing the clinical and social models which currently operate. What this means is that there could be no access to the key services that are well-positioned to provide access for the individual to his or her independence, recovery and self-development.
The providers who currently enable access to mainstream life for people with mental health conditions will need to introduce themselves to the GP consortia as a matter of urgency. In order to become better placed to continue the work of mainstream recovery it will be important to do this now. Commercial and private providers are already muscling in on the GP consortia and it is unlikely that these groups will have any expertise at all in providing hope and aspiration for marginalised people.
business,social inclusion
bridge building for mainstream,
care,
recovery
Friday, 4 March 2011
What does Pat Deegan mean by 'a career in mental health'?
When Dr. Pat Deegan coined the phrase 'a career in mental health' she was referring to endemic features of the mental health system prevailing at the time when she was first clinically diagnosed. A 'career in mental health' was the path that her specialists advised would become her future. It would mean a life on benefits, no chance of employment and massively limited access to opportunities. It would mean an end to her aspirations, and end to her hopes. Effectively, the end of a career.
For people who have been through secondary mental health experiences in the UK, a 'career in mental health' can still be the norm. Huge inroads have been made nonetheless. The recovery programmes that have been set up by many clinical teams all around the country. The user-led services that are widely encouraged and supported. The involvement in recruiting people who have experienced mental health conditions for employment within services. The movement from supported accommodation to independent living. The emphasis on mainstream by third-sector organisations working alongside the NHS and statutory services. The 'paths to personalisation' programme and the independence-based use of direct payments and personal budgets.
All of these initiatives and more are continuing to help enable people with severe and enduring diagnoses to find personal autonomy and make a break from the pitifully bleak reality of Deegan's appositely-described 'career in mental health'.
But what of the future?
In the UK we are witnessing the root-and-branch dismantling of mental health services as they currently stand. There will be no more primary care teams and more and more people are being discharged from CMHTs (Community Mental Health Teams). Within two years consortia of GPs and general practice surgeries will become the budget-holders both for primary and secondary mental health care.
At this stage there is no way of telling whether these changes will be for the better or for the worse. The only implacable fact is change itself and that changes are going to be massive and across the board.
The fallout from the first tremors of change is already with us. The much-vaunted personalisation programme was due to be rolled out universally throughout the UK within 18 months. Now I feel it is unlikely to happen at all. Personal budgets could well be forgotten in the midst of the general upheaval of services. Certainly, direct payments for mental health have become a thing of the past, at least in the south-west London borough where I work as a bridge builder. This is despite service users having a legal right to direct payments where these can be shown to be a strong factor in their recoveries.
The experience of personalisation in other parts of the UK may well be different and could paint a much more hopeful picture. Unfortunately, it won't last.
For people who have been through secondary mental health experiences in the UK, a 'career in mental health' can still be the norm. Huge inroads have been made nonetheless. The recovery programmes that have been set up by many clinical teams all around the country. The user-led services that are widely encouraged and supported. The involvement in recruiting people who have experienced mental health conditions for employment within services. The movement from supported accommodation to independent living. The emphasis on mainstream by third-sector organisations working alongside the NHS and statutory services. The 'paths to personalisation' programme and the independence-based use of direct payments and personal budgets.
All of these initiatives and more are continuing to help enable people with severe and enduring diagnoses to find personal autonomy and make a break from the pitifully bleak reality of Deegan's appositely-described 'career in mental health'.
But what of the future?
In the UK we are witnessing the root-and-branch dismantling of mental health services as they currently stand. There will be no more primary care teams and more and more people are being discharged from CMHTs (Community Mental Health Teams). Within two years consortia of GPs and general practice surgeries will become the budget-holders both for primary and secondary mental health care.
At this stage there is no way of telling whether these changes will be for the better or for the worse. The only implacable fact is change itself and that changes are going to be massive and across the board.
The fallout from the first tremors of change is already with us. The much-vaunted personalisation programme was due to be rolled out universally throughout the UK within 18 months. Now I feel it is unlikely to happen at all. Personal budgets could well be forgotten in the midst of the general upheaval of services. Certainly, direct payments for mental health have become a thing of the past, at least in the south-west London borough where I work as a bridge builder. This is despite service users having a legal right to direct payments where these can be shown to be a strong factor in their recoveries.
The experience of personalisation in other parts of the UK may well be different and could paint a much more hopeful picture. Unfortunately, it won't last.
business,social inclusion
aspiration,
bridge building for mainstream,
health,
mental health,
recovery
Friday, 8 October 2010
How mainstream is roadblocked
For many years mainstream has been perceived and practised as a key component of the care pathway in mental health provision.
At several stages of the pathway into mainstream there are roadblocks. These can occur from the individual client, from services, even from families and carers. An individual can feel apprehensive of stepping over the threshold into mainstream activities. This can be for a variety of reasons, ranging from self-stigma or from being so long in the mental health system that independence seems a very distant option. Contrary to some current opinion, it is not stigma from mainstream society that creates the main roadblock.
Dr. Pat Deegan's belief is that too often the health system can encourage what she calls 'a career in mental health' and nothing else. This viewpoint is based on her experience as a service user and it still holds true.
A great deal is being achieved by service users themselves to challenge the roadblocks. This is particularly true where creative and personalised use of direct payments and individual budgets have really taken off around the UK. It hasn't happened everywhere but some immensely inspiring stories and testimonials can be viewed at the NMHDU website.
Creative use of direct payments in mental health recovery is currently sporadic. The intention was that this should increase towards full implementation of the personalisation programme. Invididual budgets were scheduled to become the engine for much healthcare practice all over the UK by 2013. However, this is now completely overshadowed and possibly lost permanently, in the thrust towards GP consortia and budget management.
Alongside the sudden disappearance of direct payments is the disappearing access to therapies, both for primary and secondary care patients. Secondary care clients have often lost out in the therapies scenario for a variety of reasons. But clients in primary care are still entitled to a reasonably smooth road to psychological therapies. Entitlement does not ensure that those therapy services are available and in practice these too are disappearing along with personalisation and individual budgets.
Of course any client is free to fund their own mainstream recovery pathway and many do. The outcomes in this area alone (south-west London) have often been formidable. A composer who has funded her own recordings and launches now has self-employment through her music. Many are those who have accessed adult education courses and further training. Individuals have re-accessed faith venues which they had previously felt unable to enter for many years.
Not all these initiatives require direct payments - anyway those have now dried up. Many activities are free to access or funded by individual clients from their own pockets. Where direct payment has been needed it has often made the crucial difference.
Third-sector organisations also do great work in promoting access to mainstream through a variety of initiatives. 'Emergence' is an arts group run by and for service users who are also visual artists. In London and around the country 'Emergence' has pioneered access to visual arts as well as giving a platform for creativity and exhibition spaces for artists with personality disorder.
'Imagine' in south west London and Surrey also promotes a variety of arts opportunities including music production and visual arts. These are open to service users but take place in mainstream settings.
Mainstream environments have their own health, safety and insurance policies. As a consumer, the service user to entitled to the protection of these policies along with every other mainstream customer and client.
At several stages of the pathway into mainstream there are roadblocks. These can occur from the individual client, from services, even from families and carers. An individual can feel apprehensive of stepping over the threshold into mainstream activities. This can be for a variety of reasons, ranging from self-stigma or from being so long in the mental health system that independence seems a very distant option. Contrary to some current opinion, it is not stigma from mainstream society that creates the main roadblock.
Dr. Pat Deegan's belief is that too often the health system can encourage what she calls 'a career in mental health' and nothing else. This viewpoint is based on her experience as a service user and it still holds true.
A great deal is being achieved by service users themselves to challenge the roadblocks. This is particularly true where creative and personalised use of direct payments and individual budgets have really taken off around the UK. It hasn't happened everywhere but some immensely inspiring stories and testimonials can be viewed at the NMHDU website.
Creative use of direct payments in mental health recovery is currently sporadic. The intention was that this should increase towards full implementation of the personalisation programme. Invididual budgets were scheduled to become the engine for much healthcare practice all over the UK by 2013. However, this is now completely overshadowed and possibly lost permanently, in the thrust towards GP consortia and budget management.
Alongside the sudden disappearance of direct payments is the disappearing access to therapies, both for primary and secondary care patients. Secondary care clients have often lost out in the therapies scenario for a variety of reasons. But clients in primary care are still entitled to a reasonably smooth road to psychological therapies. Entitlement does not ensure that those therapy services are available and in practice these too are disappearing along with personalisation and individual budgets.
Of course any client is free to fund their own mainstream recovery pathway and many do. The outcomes in this area alone (south-west London) have often been formidable. A composer who has funded her own recordings and launches now has self-employment through her music. Many are those who have accessed adult education courses and further training. Individuals have re-accessed faith venues which they had previously felt unable to enter for many years.
Not all these initiatives require direct payments - anyway those have now dried up. Many activities are free to access or funded by individual clients from their own pockets. Where direct payment has been needed it has often made the crucial difference.
Third-sector organisations also do great work in promoting access to mainstream through a variety of initiatives. 'Emergence' is an arts group run by and for service users who are also visual artists. In London and around the country 'Emergence' has pioneered access to visual arts as well as giving a platform for creativity and exhibition spaces for artists with personality disorder.
'Imagine' in south west London and Surrey also promotes a variety of arts opportunities including music production and visual arts. These are open to service users but take place in mainstream settings.
Mainstream environments have their own health, safety and insurance policies. As a consumer, the service user to entitled to the protection of these policies along with every other mainstream customer and client.
business,social inclusion
direct payments,
mainstream,
recovery
Wednesday, 18 August 2010
Friday, 30 July 2010
Sunday, 25 July 2010
Mainstream - the Cascade Effect
As a social inclusion bridge builder I work with clients with severe and enduring mental health diagnoses. They are referred or they self-refer with the desire to access mainstream life domains.
Clients aspire to a variety of mainstream choices. It might be volunteering or befriending, it may be arts activities, it might be employment or running your own business. Client aspirations may include sports, faith, education, training or a selection from any or all of these.
Enabling individuals with a 'severe and enduring' background is not always a straightforward process although it certainly can be sometimes. A client can be introduced to a mainstream outlet and it can work for him or her almost immediately. Other clients may be unready for mainstream for a variety of reasons. They may suffer a relapse before accessing the mainstream environment. They may visualise mainstream as another form of day service or statutory support system, which it isn't.
Equally, clients can sometimes express a wish to access mainstream out of a misplaced fear that not accessing it might in some way affect their payments and benefits. It can be a long process before the value and rewards of mainstream are understood.
What is true is that clients who successfully access or re-access mainstream in turn become examples of mainstream's effectiveness. Signposting to mainstream as part of the mental health recovery pathway is undoubtedly effective, even if it does not work for everyone straight away.
Mainstream also helps to sustain recovery in the individual and even better, it can propagate more success and recovery out of its own resources. An example of this would be the musician who successfully links up with a mainstream recording studio. After months of regular rehearsal the musician is invited by the studio manager to contribute to a recording session. I witness this kind of beautiful outcome and its benefits for the client in my work as an arts bridge builder.
Another example - again from music bridge building - is the guitarist client who uses a studio regularly and invites a friend to join him during the session. The friend may well be another mental health service user who has never successfully engaged with mainstream despite the best efforts of the bridge building service. Where services have been unsuccessful a friendship and peer network can do the job far more effectively.
Mainstream reaches the places other services cannot reach and in the process it is able to create a cascade effect - a continuing path of development, recovery and individual growth.
Clients aspire to a variety of mainstream choices. It might be volunteering or befriending, it may be arts activities, it might be employment or running your own business. Client aspirations may include sports, faith, education, training or a selection from any or all of these.
Enabling individuals with a 'severe and enduring' background is not always a straightforward process although it certainly can be sometimes. A client can be introduced to a mainstream outlet and it can work for him or her almost immediately. Other clients may be unready for mainstream for a variety of reasons. They may suffer a relapse before accessing the mainstream environment. They may visualise mainstream as another form of day service or statutory support system, which it isn't.
Equally, clients can sometimes express a wish to access mainstream out of a misplaced fear that not accessing it might in some way affect their payments and benefits. It can be a long process before the value and rewards of mainstream are understood.
What is true is that clients who successfully access or re-access mainstream in turn become examples of mainstream's effectiveness. Signposting to mainstream as part of the mental health recovery pathway is undoubtedly effective, even if it does not work for everyone straight away.
Mainstream also helps to sustain recovery in the individual and even better, it can propagate more success and recovery out of its own resources. An example of this would be the musician who successfully links up with a mainstream recording studio. After months of regular rehearsal the musician is invited by the studio manager to contribute to a recording session. I witness this kind of beautiful outcome and its benefits for the client in my work as an arts bridge builder.
Another example - again from music bridge building - is the guitarist client who uses a studio regularly and invites a friend to join him during the session. The friend may well be another mental health service user who has never successfully engaged with mainstream despite the best efforts of the bridge building service. Where services have been unsuccessful a friendship and peer network can do the job far more effectively.
Mainstream reaches the places other services cannot reach and in the process it is able to create a cascade effect - a continuing path of development, recovery and individual growth.
business,social inclusion
arts,
growth,
mainstream,
music,
recording,
recovery,
self-development
Tuesday, 13 July 2010
History of Social Inclusion
Social Inclusion and mainstream arise out of a history and out of a history of ideas.
Government think-tanks in the late 1990s and early 2000s had a key role in developing current thinking and practice around social inclusion. The envisaging of 'social domains' relevant to people's lives arises from these seminal ideas. The role of mainstream bridge builder is also developed around the concept of mainstream as a pathway for mental health recovery.
Social Inclusion goes back even further. A single act of defiance by Rosa Parks in 1955 in Alabama Mississippi. A black woman refusing to give up her seat on the bus to a white person, thereby defying the segregration laws. A key moment that lies at the heart of the civil rights movement, not just for the United States but for equality and social inclusion everywhere.
Equal opportunities, diversity, social inclusion and fairness are now commonplaces, enshrined in the way we strive to live and work today.
Government think-tanks in the late 1990s and early 2000s had a key role in developing current thinking and practice around social inclusion. The envisaging of 'social domains' relevant to people's lives arises from these seminal ideas. The role of mainstream bridge builder is also developed around the concept of mainstream as a pathway for mental health recovery.
Social Inclusion goes back even further. A single act of defiance by Rosa Parks in 1955 in Alabama Mississippi. A black woman refusing to give up her seat on the bus to a white person, thereby defying the segregration laws. A key moment that lies at the heart of the civil rights movement, not just for the United States but for equality and social inclusion everywhere.
Equal opportunities, diversity, social inclusion and fairness are now commonplaces, enshrined in the way we strive to live and work today.
business,social inclusion
business,
recovery,
Rosa Parks,
social inclusion
Friday, 21 May 2010
Recovery
Recovery
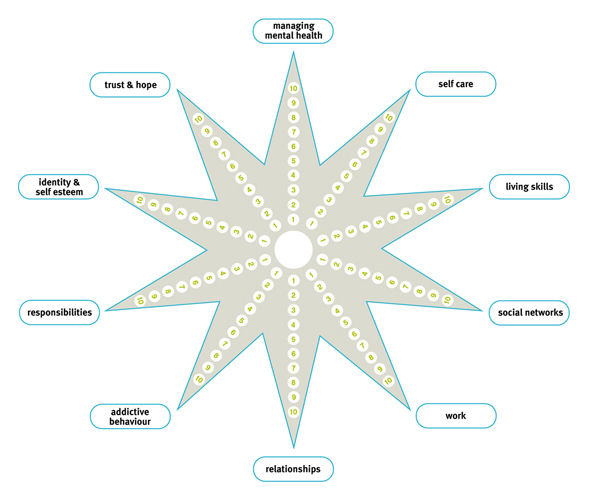
Recovery is a process of hope and aspiration that signals the return to mainstream life for those who have experienced mental health problems. Recovery can take place regardless of whether the individual is symptom-free or not. Hope and recovery are recognised as key parts of the care pathway. Social inclusion bridge builders work with clients on a recovery programme based on the client's own choices and aspirations.
More about Recovery and the work of Dr. Pat Deegan
Recovery is a process of hope and aspiration that signals the return to mainstream life for those who have experienced mental health problems. Recovery can take place regardless of whether the individual is symptom-free or not. Hope and recovery are recognised as key parts of the care pathway. Social inclusion bridge builders work with clients on a recovery programme based on the client's own choices and aspirations.
More about Recovery and the work of Dr. Pat Deegan
business,social inclusion
aspiration,
inclusion,
pat deegan,
recovery
Subscribe to:
Posts (Atom)